Key Takeaways
- Accurate data migration prevents denied claims and payment delays.
- Clearinghouse transitions can cause cash flow disruptions if mishandled.
- Proper staff training reduces surgical billing errors and ensures revenue continuity.
- Explore billing services specifically designed for surgical practices.
Have you ever upgraded your smartphone software, expecting better speed, smarter design, and smoother navigation only to feel frustrated when data doesn’t transfer correctly and apps malfunction? Now imagine that kind of disruption—only in your surgical practice’s billing department.
Switching to a new surgery EHR can streamline documentation, enhance patient care, and allow your team to adopt processes that enhance their workflows. However, without careful planning, it may also introduce medical billing errors, delayed payments, and compliance headaches.
If you’ve made the decision to implement a new EHR, avoid the following common billing mistakes so your practice’s financial performance doesn’t suffer during the transition.
Table of Contents
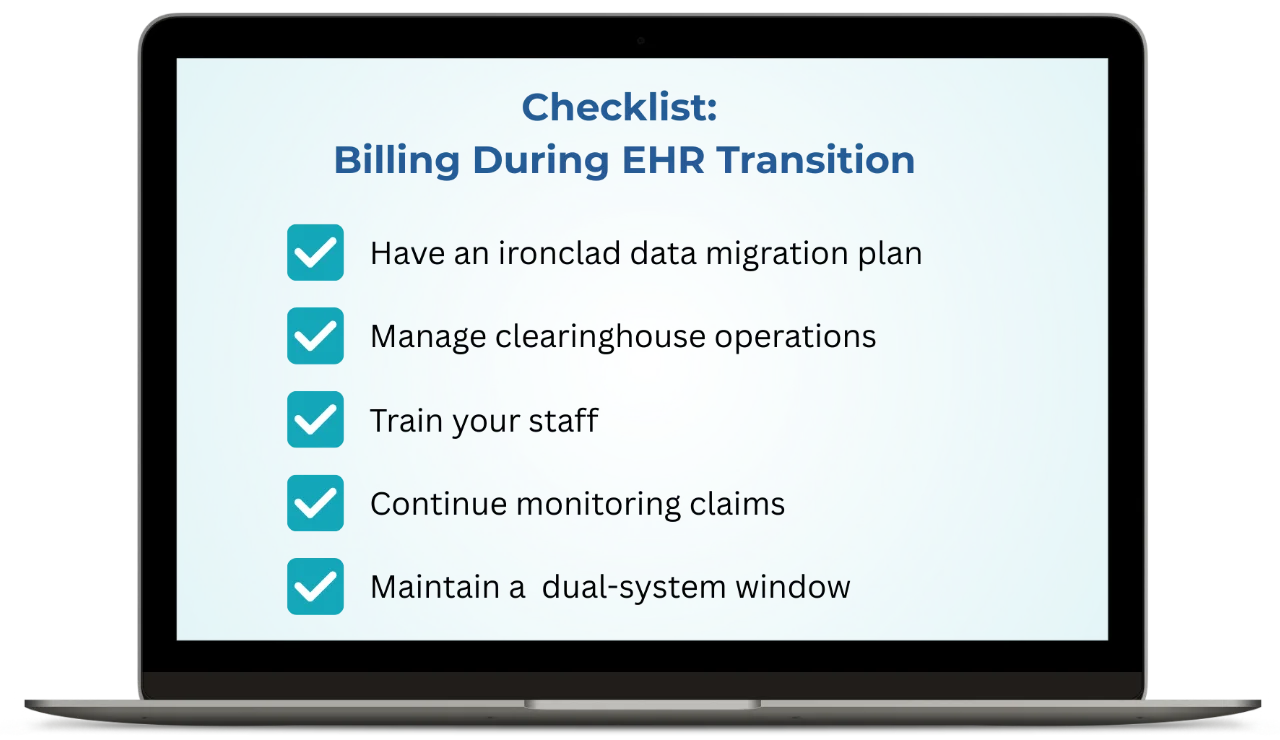
1. Forgetting Data Migration and Validation Steps
The transition to a new surgery EHR carries serious risks if billing data isn’t migrated properly. Missing or corrupted records may leave your practice scrambling to deal with denied claims, incorrect balances, and extended payment delays. When switching EHRs, many teams overlook the need to transfer complete financial data—including patient history, unpaid claims, payer contracts, and aged reports.
According to a study published in the Journal of the American Medical Informatics Association, nearly 38% of healthcare data migration projects exceed budgets or encounter delays due to preventable issues. Without a detailed plan, surgical practices can face long-term revenue challenges.
How to Avoid It
Collaborate with a specialty-specific EHR vendor to create a comprehensive data migration strategy. Before going live, validate all transferred billing records. Submit test claims and audit migrated data to spot discrepancies early. When you start using the new system, use a small group of live claims initially, and then launch the full rollout to minimize financial risk.
2. Ignoring Clearinghouse Transitions
Changing EHRs often disrupts internal communication in your organization, and is another reason surgery practices struggle with medical billing errors during an EHR transition. The American Medical Association reports that disrupted health information exchanges during EHR changeovers can create obstacles to communication and data flow, and it’s wise to remain attentive to all parties involved, including clearinghouses.
Switching to a new surgery EHR often impacts how claims are submitted and payments are received. Failing to notify payers or update enrollment data can disrupt claim processing and delay reimbursements. Clearinghouse changes also affect ERA (Electronic Remittance Advice) workflows and payment postings. If overlooked, shifts in clearinghouse communications can generate administrative backlogs and lead to missed revenue.
How to Avoid It
Notify all payers about your EHR transition well in advance. Update clearinghouse enrollment details and verify integrations with the new surgery EHR. Collaborate with your vendor to ensure smooth claims flow. Closely monitor submissions during the early stages and maintain backup workflows in case of interruptions.
3. Insufficient Training for Surgical Billing Staff
No matter how advanced your new system is, undertrained staff can derail your billing process. Errors like missed modifiers, incorrect CPT codes, or partial claim entries can reduce reimbursement and trigger audits.
In surgical settings—where billing often involves multiple procedure codes, assistants, and facility fees—accuracy is crucial. Lack of proper training may also result in violations of insurer or regulatory documentation rules.
How to Avoid It
Invest in thorough, role-based training for your billing team before the go-live date. Your EHR vendor can create a custom training plan that best fits your practice’s structure, including hands-on workshops, quick-reference guides, and post-launch support. Designate “super-users” to help colleagues troubleshoot as they adapt to the new system and regularly review compliance changes that may impact billing practices.
4. Failing to Monitor Claims When Switching EHRs
When switching to a new surgery EHR, it’s easy to get caught up in setup tasks and unintentionally let active claims fall off the radar. But keeping an eye on those claims is crucial—otherwise, denials can start to pile up and deadlines might slip by, cutting into revenue and increasing workload.
Plus, changes in how the new system handles coding or claim batching can introduce small errors that may go unnoticed without regular check-ins. Without early and consistent oversight, these small issues can quietly escalate into larger RCM problems.
How to Avoid It
Assign billing personnel to manage claims across both the old and new systems during the transition. Run dual reports and use analytics to identify variances in reimbursement or claim rejection rates. Establish workflows to quickly address denials and resubmit problematic claims.
5. Skipping a Dual-System Window
Shutting down your old EHR too soon can lead to unintended revenue loss and unexpected bumps in the road. Without access to historical data, billing teams may struggle to verify older claims or handle post-payment audits. It’s important to confirm that the new system is accurate and smoothly operating before fully relying on it.
Maintaining both systems during the early phases is like using a safety net. It helps your team double-check records, confirm balances, and catch any issues before they affect your revenue.
How to Avoid It
Keep both systems active for 60–90 days after the new surgery EHR goes live. This overlap allows your team to follow up on legacy claims, track discrepancies, and ensure seamless billing continuity. Preserve read-only access to your old system for longer if needed for audits or payer requests.
This system is amazing. It gives you the peace of mind that none of the information will be lost.
Cristina Garcia, Practice Manager, Ricardo Calonge M.D.
Experience a Smooth Transition
Your EHR transition doesn’t have to disrupt your surgical billing workflows. By avoiding these five common errors, your practice can maintain revenue integrity while reaping the full benefits of a new system. A specialty-specific vendor, focused planning, proper training, and continuous claim monitoring can make all the difference during implementation.